Proliferation of State-Level AI Laws, Medical Coding Automation, Disappearing MA Plans, Google Quantum Advantage, and More
This article explores the rapidly evolving landscape of AI in healthcare and technology, highlighting the proliferation of state laws governing AI, the current state and future of medical coding automation, and the resilience of major EHR vendors amid disruptive innovation. It discusses how new regulations are shaping AI’s role in healthcare, with specific state provisions impacting medical decision-making and patient interactions. The piece also examines the financial challenges facing Medicare Advantage plans and provides insights into Google’s recent quantum supremacy announcement, emphasizing its significance for computing and security.
Joe Bastante
10/30/20256 min read

In this update:
State laws governing AI, what to know
Medical coding with AI, are we there yet?
Will EHR vendors be disrupted by tech-savvy innovators?
Where have all the Medicare Advantage plans gone, should I be worried?
What to make of Google's quantum supremacy announcement
State laws governing AI, what to know
The One Big Beautiful Bill Act failed in introducing a moratorium on state or local regulation of AI. State and local regulations continue to proliferate. The good news for those building or using AI solutions is that most states haven't passed overly restrictive AI legislation. The bad news is that hundreds of regulations enacted or in-flight across the states have implications for AI. For those states with key AI legislation, requirements often center on reporting and disclosure, testing and avoidance of bias, and establishment of controls. Some states have healthcare-specific provisions, e.g., Arizona requires medical professionals (not AI) to make final decisions on claims denials, Illinois disallows any AI-driven service from providing mental health decision-making, Nevada has similar provisions, Utah requires disclosure to patients when using AI, and Texas also requires disclosure of AI use and requires medical professional reviews in certain cases. Check out the link below to get a sense of how many states have passed health-related AI laws.
What makes AI regulation complicated are AI-related clauses in bills that are not explicitly targeted at AI. Everything from budget to child pornography bills have included AI provisions. For example, in California, bills related to consumer protection, digital replicas, political advertising, employment and contracting, and healthcare services include provisions related to AI. Even cities are enacting AI laws. For example, Jersey City (NJ) and San Francisco ban use of AI and algorithms for setting rent prices. The moral of the story is that, while AI legislation is often mentioned in the news, popular news sources don't begin to cover all of the relevant regulations. Check out the links below if you need complete information.
Two sites providing a comprehensive list of state-level AI legislation:
https://www.ncsl.org/technology-and-communication/artificial-intelligence-2025-legislation
List of states with health AI policies:
https://www.manatt.com/insights/newsletters/health-highlights/manatt-health-health-ai-policy-tracker
Medical coding with AI, are we there yet?
Administrative activities in healthcare cost roughly $600 billion to $1 trillion annually in the U.S. Medical coding and related processes are a significant component of that cost (roughly 15-20%). Provider, payers, and government organizations all code to standardized code sets like ICD-10, CPT, and HCC. About a year ago, I predicted that we'd start seeing AI-enabled coding picking up momentum in about 18 months (i.e., early 2026) and taking a couple more years to become common. We're right on track. A few takeaways...
First, usability and integration with EMRs and other core systems is arguably the most important consideration. At present, AI is best suited to improve human productivity rather than replace humans. Early evidence suggests human coding efficiency can be doubled and made more accurate using AI. AI coding accuracy varies widely, though can be 99% or higher when models are tuned for narrow specialties. Common areas of use are radiology and emergency departments, with successes in specialties like nephrology. The vendor landscape is complex ranging from large healthcare tech vendors (Optum, 3M), specialty tech companies (Nym, Fathom, and CodaMatrix), and smaller hopefuls (Maverick Medical AI, BUDDI.AI, Arintra, etc.). Ultimately, this capability will be provided by EHR vendors, so successful tech companies stand a good chance of being acquired or run out of town. So, are we there yet? Well, we've arrived at the amusement park but most of the rides are still under construction.
Quick read on the medical coding market:
https://www.snsinsider.com/reports/ai-driven-medical-coding-market-7729
KLAS on coding technology vendors (for-pay report, but you can find summaries online or download it from vendors scoring high on the report like Fathom):
https://klasresearch.com/report/autonomous-coding-2025-a-promising-start-for-an-early-market/3166
Will EHR vendors be disrupted by tech-savvy innovators?
This question has come up a couple times for me recently. With all the innovative companies moving traditional provider processes to AI-centric workflows, will this disrupt the big EHR vendors? No. For the longer answer, there's been a continuous stream of innovation by vendors looking to make EHR-related processes more efficient and modern. For example, in the last week or so, stories were published. e.g., Optum's new Optum Real, which uses AI to reduce claims denials and improve prior authorization. Humata Health also announced streamlined prior authorization, built on top of Microsoft Dragon Copilot, which extends EHRs. Speaking of Microsoft Dragon Copilot, Microsoft also just announced extending workflows for nurses by integrating AI agents.
Some may see this as a continuing trend of innovation with AI and agents ultimately obviating the need for EHRs. This is unlikely for a few reasons. First, we're nowhere ready to replace EHRs systems with agents. As we covered above, laws are becoming more common, which prevent AI autonomy and decisioning in healthcare. The cost of replacing EHR systems is very high and not an attractive option. EHR vendors (Epic, Oracle, Meditech, etc.) continue to add their own AI capabilities. Large EHR vendors can simply buy AI innovators (though Epic normally doesn't). EHRs serve as essential plumbing for business operations, including integration with other providers, payers, and regulators. They also serve as patient engagement platforms. There are many other reasons, but you get the picture. Innovators may be moving quickly, but EHR vendors are in the hunt.
Microsoft 's announcement regarding Dragon Copilot for nurses is worth a read:
Check out Epic's AI page, they're adapting quickly:
Where have all the Medicare Advantage plans gone, should I be worried?
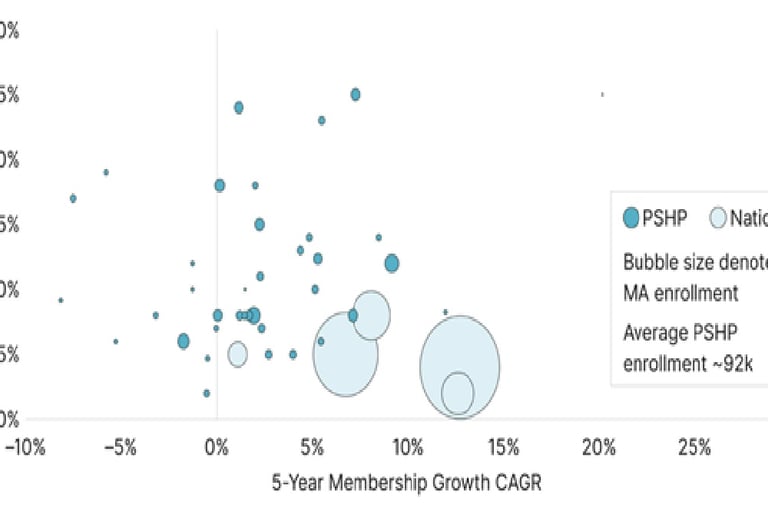
The past two years have been financially difficult for Medicare Advantage plans. If you recall an earlier post of mine, many insurers reduced the number counties and states in which they offer MA plans. In 2024, MA plans had a combined underwriting loss of $5.7 billion. While the CMS increased the average reimbursement rate by over 5% for 2026, this is likely insufficient for many insurers. Not all states will see a reduction in plans, though 35 states, DC, and Puerto Rico will have fewer plans. On a positive note, CMS noted that the average monthly premium across MA including special needs plans will decrease from $16.40 in 2025 to $14.00 in 2026. This may not be enough stave off MA enrollment decreases, which are projected to shrink from 34.9 million in 2025 to 34 million in 2026.
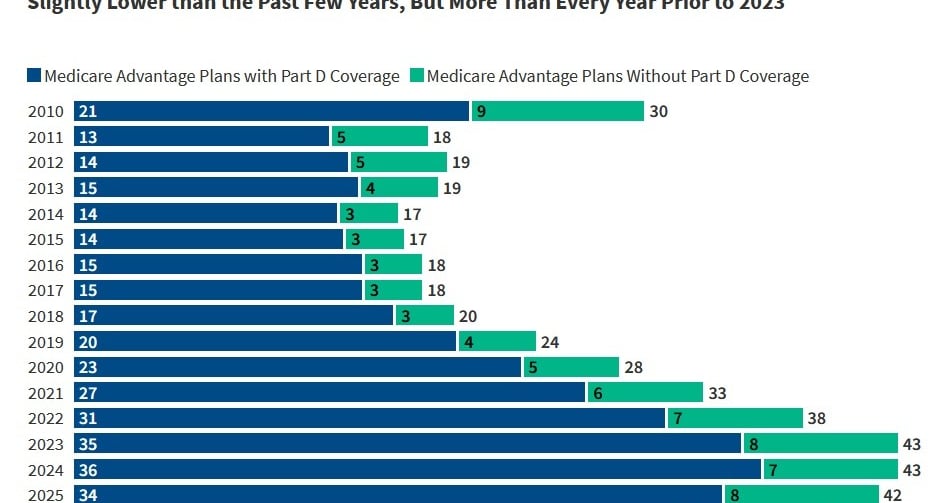
Should those who depend on MA be concerned? Not yet. While the number of MA plans have been decreasing since 2024, we're roughly at the 2022 levels. However, some states and counties will be disproportionately impacted. In renewing 2026 MA benefits for my parents, they number of plans in their town dropped dramatically, down to only 6 and only one PPO plan. Check out the chart below from KFF on the average number of MA plans available.
Research from KFF and Oliver Wyman:
What to make of Google's quantum supremacy announcement
You may have seen the headlines, e.g., from ComputerWorld, Google’s Quantum chip claims 13,000x speed advantage over supercomputers. I've written on quantum computing before given the concerns it raises about cyber and national security. First, let me summarize what Google's achievement means for most of us: Google has made an impressive step forward in demonstrating quantum's performance supremacy over traditional computers for a single algorithm, yet this is one of many steps that must be taken before quantum computing is ready for broad application.
What they did: they implemented the Quantum Echoes algorithm, which runs an operation across the system's qubits, then introduces a change to one of the qubits, then runs the process in reverse to return the system to the starting point (except for the impact of the single changed qubit). The starting and ending calculations ought to be the same except for the measurable impact of the changed qubit.
Why does this matter: To begin with, this algorithm has practical applications, for example, simulating the interactions within molecules (think material science and drug discovery) and simulating black hole dynamics. Second, they demonstrated a 13,000 times performance advantage over classical computers for this algorithm. Finally, Google demonstrated a low error rate and measurement repeatability, which were major achievements for quantum computing.
While these results are impressive, they are but one step toward the commercial deployment of quantum computers.
Check out this well-written article if you'd like more information:
https://ki-ecke.com/insights/quantum-echoes-algorithm-explained-how-it-reveals-structure/
As always, feedback, suggested topics, or questions are welcomed. I’m here to help. Contact me anytime.
Contact us
Whether you have a request, a query, or want to work with us, use the form below to get in touch with our team.